Navigating Humana Medicare Prior Authorization for Radiology
Imagine needing an MRI. You've consulted your doctor, scheduled the appointment, and are ready for answers. Then, a roadblock: Humana Medicare prior authorization for radiology. What does it mean? Why is it necessary? This seemingly complex process can be daunting, leaving patients feeling confused and frustrated. This guide will demystify Humana's pre-authorization process for radiology services, providing you with the information you need to navigate the system efficiently.
Humana Medicare prior authorization for radiology essentially means getting approval from Humana before undergoing certain imaging procedures. This process allows Humana to review the medical necessity of the requested scan, ensuring that it aligns with established guidelines and is the most appropriate course of action. This can involve anything from a basic X-ray to more complex procedures like CT scans and MRIs. While it might seem like an extra hurdle, it's designed to help manage costs and ensure patients receive the most appropriate and effective care.
The history of prior authorization is rooted in cost containment efforts within the healthcare industry. As medical technology advanced and the cost of imaging services rose, insurance companies implemented pre-authorization processes to control spending and prevent unnecessary procedures. While the specifics have evolved, the core principle remains the same: ensuring appropriate resource allocation and value-based care.
The importance of Humana Medicare pre-authorization for radiology lies in its potential to reduce healthcare costs by preventing unnecessary procedures. It also helps optimize resource utilization, ensuring that expensive imaging equipment is used judiciously. Furthermore, prior authorization can play a crucial role in patient safety by prompting a review of medical necessity, potentially identifying alternative, less invasive diagnostic options.
However, the Humana Medicare radiology pre-authorization process is not without its challenges. One of the main issues is the potential for delays in care. Obtaining pre-authorization can take time, sometimes delaying necessary treatment. This can be particularly problematic in urgent situations. Another challenge is the administrative burden it places on both healthcare providers and patients, requiring time and effort to complete the necessary paperwork and follow-up.
One benefit is cost savings for patients. By ensuring the procedure is medically necessary, it helps prevent patients from incurring costs for unnecessary tests. Another benefit is improved care coordination. The pre-authorization process fosters communication between healthcare providers and Humana, ensuring alignment on the treatment plan. Finally, it promotes evidence-based care by aligning treatment with established guidelines and best practices.
Advantages and Disadvantages of Humana Medicare Prior Authorization for Radiology
| Advantages | Disadvantages |
|---|---|
| Cost savings | Potential delays in care |
| Improved care coordination | Administrative burden |
| Promotes evidence-based care | Potential for denied claims if process isn't followed correctly |
Frequently Asked Questions:
1. What is Humana Medicare prior authorization for radiology? (Answered above)
2. How do I obtain prior authorization? Contact Humana directly or use their online portal.
3. How long does the process take? It can vary, but typically takes several business days.
4. What if my prior authorization is denied? You can appeal the decision.
5. What information do I need to provide? Medical records, diagnosis codes, and the requested procedure.
6. Are all radiology procedures subject to prior authorization? No, only certain procedures require it.
7. Can my doctor's office handle the pre-authorization process? Yes, often they will manage it for you.
8. What happens if I have the procedure without prior authorization? You may be responsible for the full cost.
In conclusion, navigating Humana Medicare prior authorization for radiology might seem complex at first, but understanding the process and its purpose can empower patients to take control of their healthcare journey. While there are challenges, the benefits of cost savings, improved care coordination, and evidence-based treatment make it a critical component of the healthcare system. By being proactive, informed, and communicating effectively with your healthcare provider and Humana, you can navigate the pre-authorization process smoothly and ensure timely access to the necessary radiology services. Remember to always check with Humana directly for the most up-to-date information and specific requirements for your plan. This proactive approach will not only facilitate the process but also contribute to better health outcomes in the long run. It's crucial for patients to understand their rights and responsibilities within the healthcare system, and understanding the pre-authorization process is a significant step in that direction.

humana medicare prior authorization radiology | Kennecott Land

Humana prior authorization form pdf Fill out sign online | Kennecott Land

19 humana forms prior authorization | Kennecott Land

Printable Humana Prior Authorization Form | Kennecott Land

Free Medicaid Rx Prior Authorization Forms | Kennecott Land
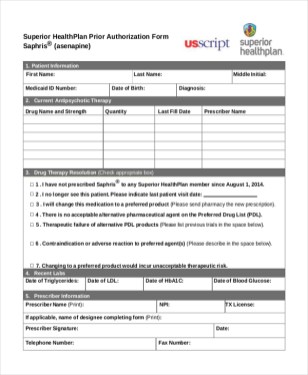
Superior Health Plan Radiology Prior Authorization Form | Kennecott Land

humana medicare prior authorization radiology | Kennecott Land

Authorization Fax Request Form | Kennecott Land

Virginia Medicaid Prior Auth Form | Kennecott Land

humana prior authorization form pdf Ten Top Risks Of | Kennecott Land

Healthfirst Leaf Plans Prior Authorization Forms | Kennecott Land

2010 Humana Military Patient Referral Authorization Form Fill Online | Kennecott Land

Free Medicare Prior Rx Authorization Form | Kennecott Land

Humana Medicare Part D Prior Authorization Forms For Medication | Kennecott Land

Medical Benefit Prior Authorization | Kennecott Land